Data-Driven Return to Activity
Earlier this year Sean Ross-Ross, Plantiga’s CTO, posted about his recovery from a right ankle fracture and syndesmotic injury he suffered in November 2019 after slipping on a wet dock. In this post, I review Sean’s Plantiga data and discuss his rehabilitation progress, 7 months later.
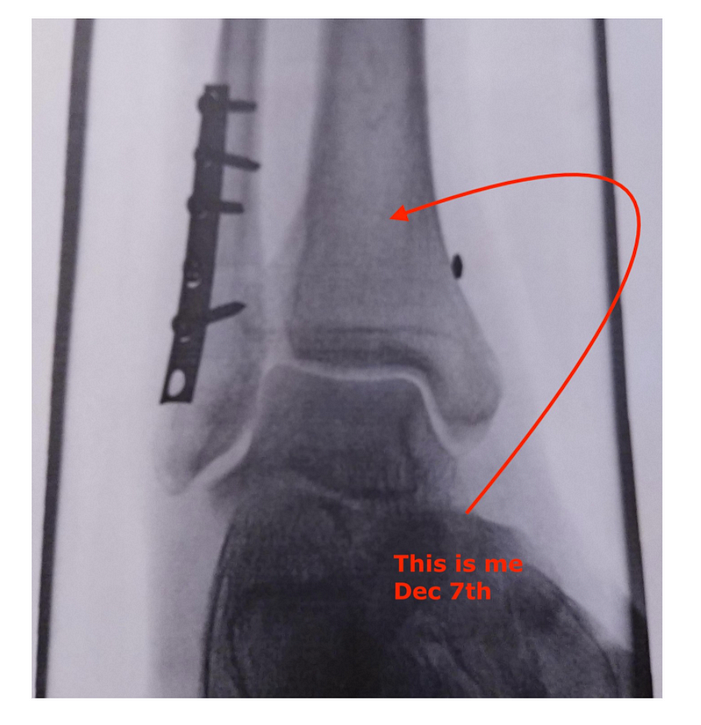
Sean’s Right Ankle
Sean underwent syndesmotic suture fixation and an open reduction and internal fixation of a right distal fibular fracture on November 9, 2019. He was placed in a walking boot cast and told not to weight-bear on the injured limb for the next 9 weeks. For those of you wondering if this was an aggressive non-weight bearing time period, it was, but it’s not uncommon for syndesmotic injuries to be immobilized for 9 to 12 weeks after surgical fixation.
On January 15th Sean’s orthopaedic surgeon allowed him to weight bear as tolerated and he was discharged to the care of his physical therapist. He had been working with them once per week to improve his ankle range of motion and strength until COVID-19 pandemic precautions limited in-person therapy mid-March. Typical rehabilitation sessions included TheraBands, calf-raises, balance-focused activities and stretches to improve his range of motion.
Admittedly when I spoke with Sean, he said his planned return to prior activities by mid-April was too ambitious. Before the ankle injury he was running 10 km every other day. His baseline Plantiga data show he was fit and had good leg strength that was symmetrical.
Baseline Plantiga Data
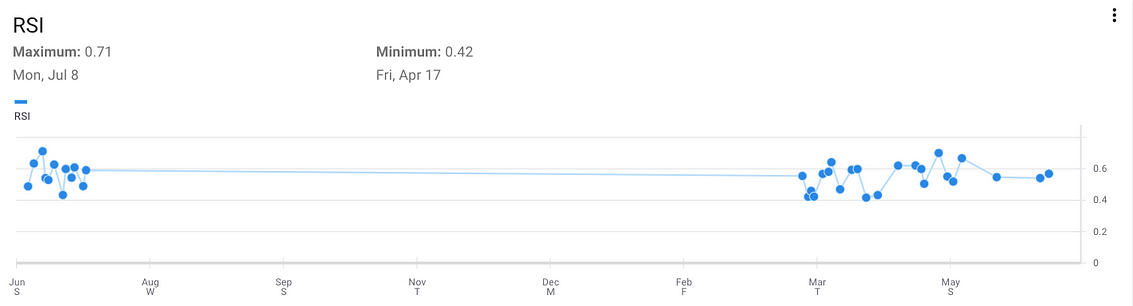
Cyclic Countermovement Jump Reactive Strength Index (CMJ RSI)
Sean’s pre-injury CMJ RSI (on the leftof the graph above) was above average compared to males in the Plantiga database. Notice how the RSI data fluctuates up and down. Plantiga’s Head of Science and Performance, Dr. Matt Jordan, tells me RSI is often used with athletes to monitor neuromuscular fatigue so as Sean’s training ramps up and he becomes fatigued, his RSI score will decrease. When he rests and recovers, his RSI will increase. This is another valuable application of the Plantiga system Dr. Jordan explains here but for now, let’s focus on his functional assessments.
On July 8, 2019 Sean had his “best” CMJ RSI of 0.71 and here’s what some of his raw jump data looks like:
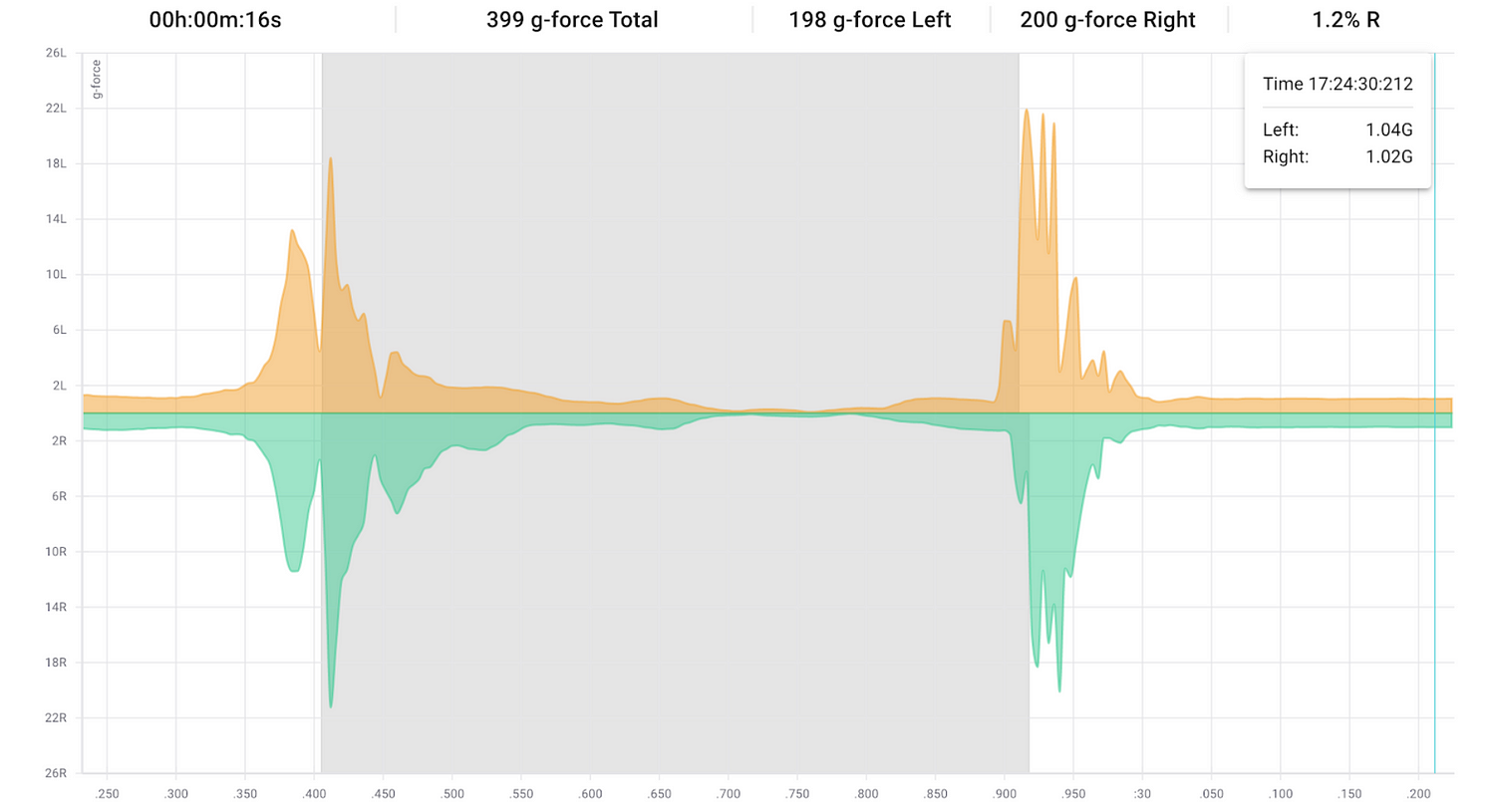
Raw Cyclic CMJ Plantiga Data
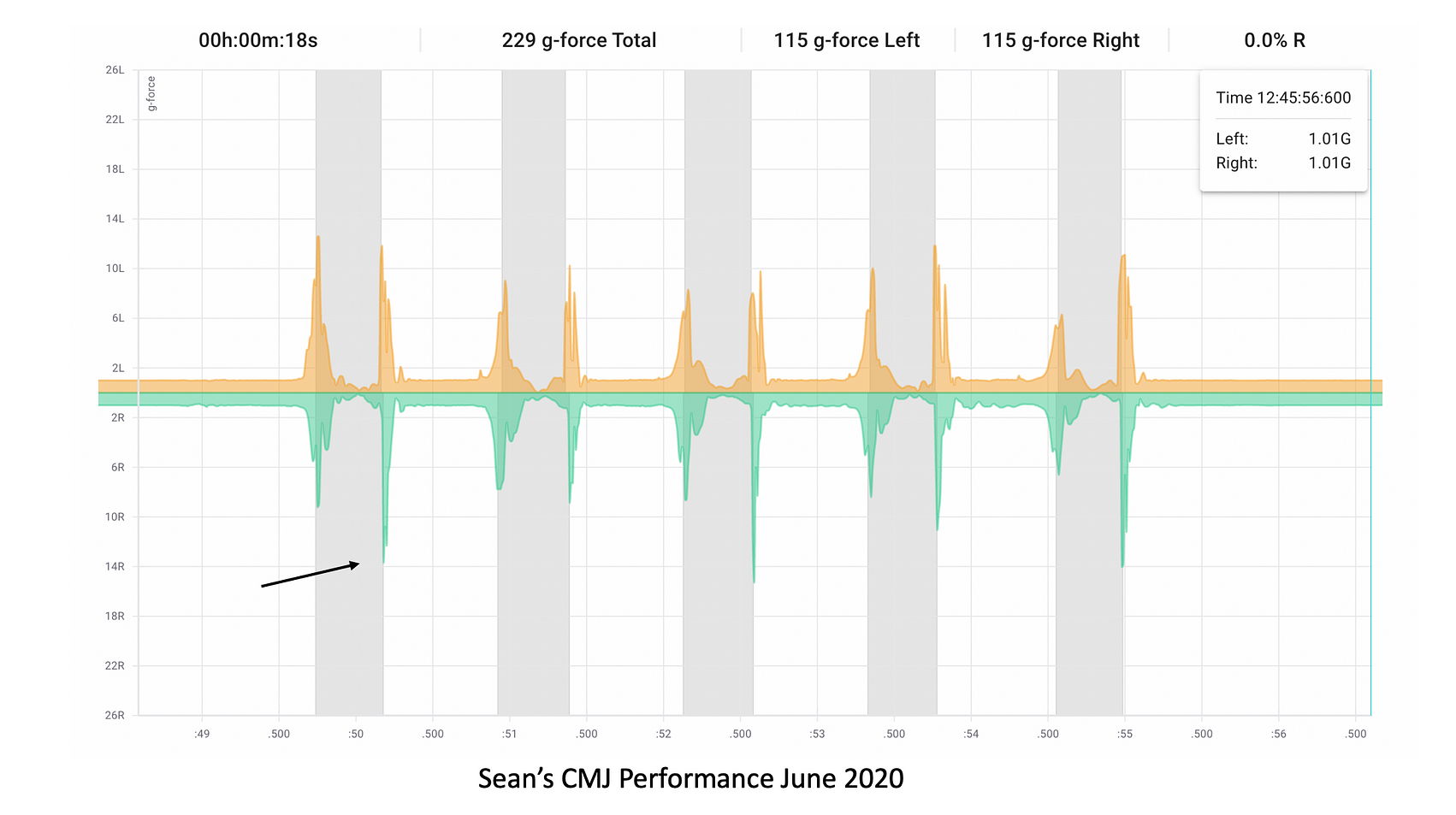
In this image, the orange tracing shows his left limb and the green tracing indicates his right limb. The takeoff for this jump is illustrated by the first series of peaks to the left of the grey band, the flight time is represented by the grey band and the landing phase is shown to the right of the grey band. Acceleration in the concentric movement phase or the propulsion phase of the jump (measured as the g-forces) shows low between-limb asymmetry. The same is true of the landing phase and his non-injured limb touches down prior to the injured limb. Peak landing forces also show low between limb asymmetry (Left 21.92G vs. Right 20.11G). Average jump height was roughly 30cm.
Rehabilitation Progress
Now seven months post-op, Sean is wondering if he’s on track to return to running and how to progress the volume and intensity of a run-walk program he’s recently started. Early in his rehabilitation, Sean was focused on improving walking speed and evaluating his side-to-side asymmetries with Plantiga. Now that his walking gait has largely normalized, it is tougher to appreciate side to side differences.
Plantiga Walk Data
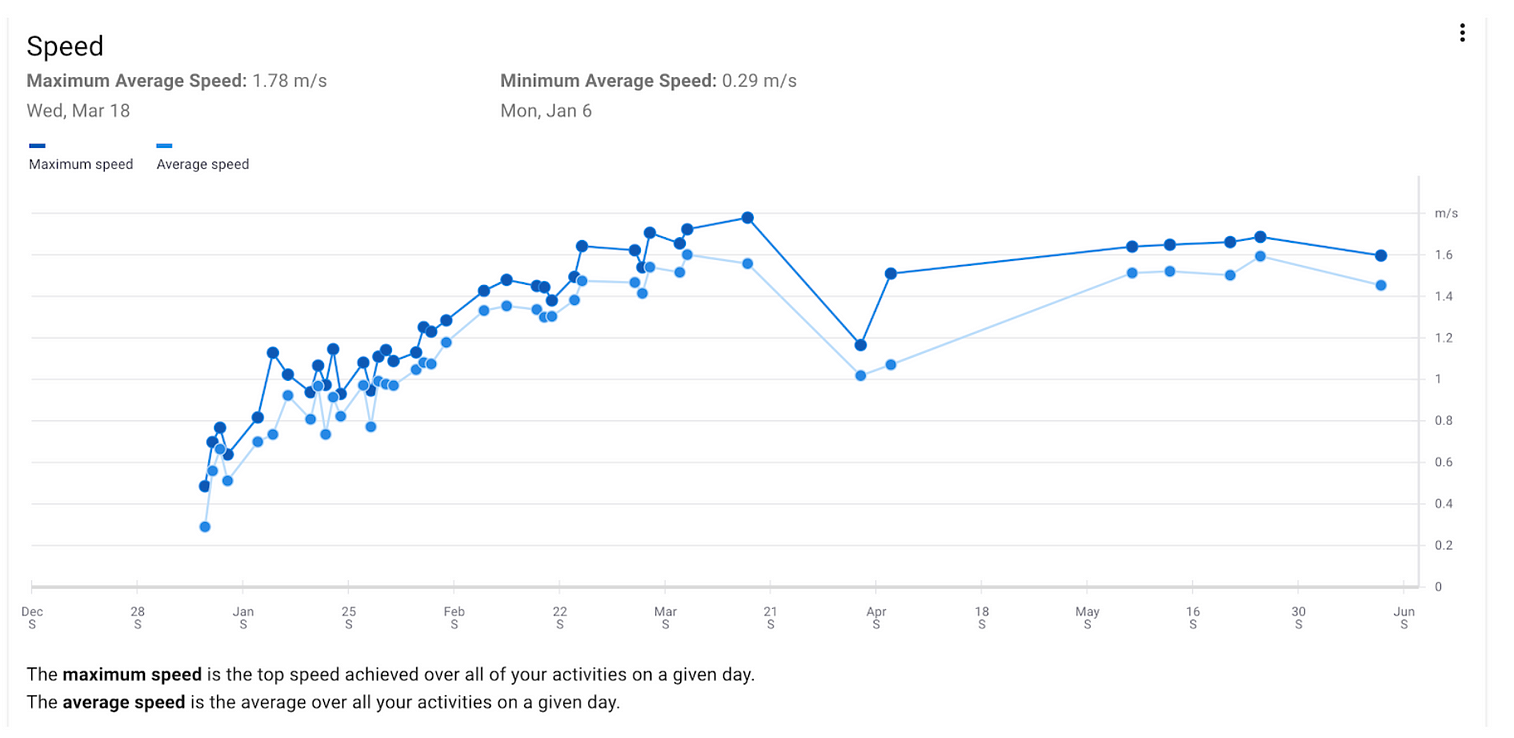
Walking Speed
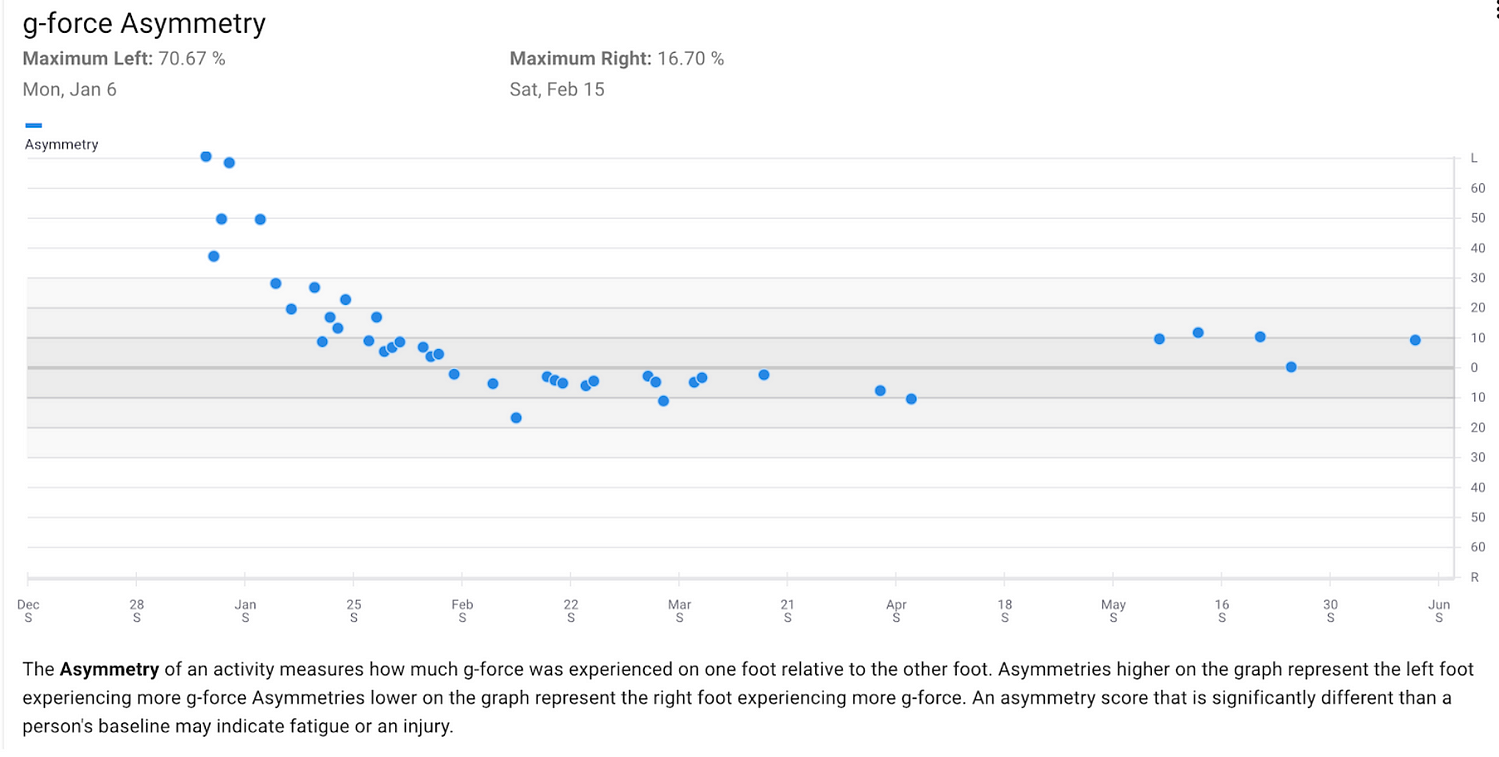
G-Force Asymmetry — Walking
In speaking with Dr. Jordan, who has been involved with the rehabilitation of many of Canada’s top high performance athletes, this is to be expected. “Rehabilitation after a lower body injury generally progresses as a progressive sequence of functional milestones. We have to re-learn how to walk before we can jog, jog before we can run, jump with two legs before we can jump with one, and put on the brakes before we can incorporate change of direction movements. The last stage would be unrestricted return to open activity, and here Plantiga provides a novel solution through its advanced movement detection capabilities that can auto-detect walking, running and jumping. This functional milestone progression and gradual reintroduction to the demands of open activity has been referred to as the control to chaos progression.”
My clinical approach as a Physical Medicine and Rehabilitation specialist to evaluating an individual’s rehabilitation progression and readiness to return to activity is first ask myself, where would I expect them to be at this point knowing the natural history of their injury and who they are as an athlete? With the Plantiga’s machine learning capabilities post-injury functional recovery curve timelines will allow us to eventually pinpoint if a patient is tracking on schedule, behind schedule or ahead of schedule based on the nature of their injury and baseline functional status. But for now we’re limited to the literature and clinical experience.
Compared to a typical ankle injury, a “high” ankle sprain with syndesmotic fracture has a prolonged recovery. In professional football players syndesmotic injury doubles an athlete’s recovery time. The gold standard treatment for an unstable syndesmotic injury is screw fixation but with that procedure patients are kept non-weight bearing longer and there is a greater risk of implant failure. Alternatively a suture button fixation device is placed across the syndesmosis, which allows for earlier rehabilitation, less risk of implant dysfunction and less risk recurrent syndesmotic widening. Functional outcomes between the two are similar. In a military population (predominantly male < 30 years of age), 81% returned to active duty and passed their physical assessment evaluations.
The proposed return to play criteria/return to activity for syndesmotic ankle injuries includes:
80–90% limb symmetry in broad (horizontal jumps)
The ability to hop on the affected side for 30 seconds pain-free.
Normal functional questionnaire scores.
Able to perform sport-specific maneuvers with good movement quality and little to no pain and instability.
Dr. Jordan tells me though that in his experience of returning individuals to pre-injury activities, cutoffs are often arbitrary and not evidence-based. For example, while a limb symmetry of 90% is often used as a threshold for return to activity, what if the patient had two symmetrical but weakened limbs? Likewise, what if they achieved a limb symmetry index of 90% for running stride length but they still had only a 75% limb symmetry index for the single leg vertical jump?
He highlights that clinicians need a battery of functional tests to pinpoint deficits and to progress the patient properly using a milestone-based approach to rehabilitation. “At the end of the day, we can’t make someone better with the right type of rehabilitation exercise if we don’t know what’s wrong, and we will never know what’s wrong if we aren’t measuring. In simple terms, you can’t change what you don’t measure, and you have to measure the things that matter!”
Sean’s Current Status (7 months post-op)
Some pain over the region of the fibular plate, usually after more dynamic activities.
Limited ankle dorsiflexion range of motion, normal plantar flexion range of motion.
Walking speed and limb symmetry at baseline.
Pain-free jumping and jogging in the sagittal plane.

Plantiga Jump Data
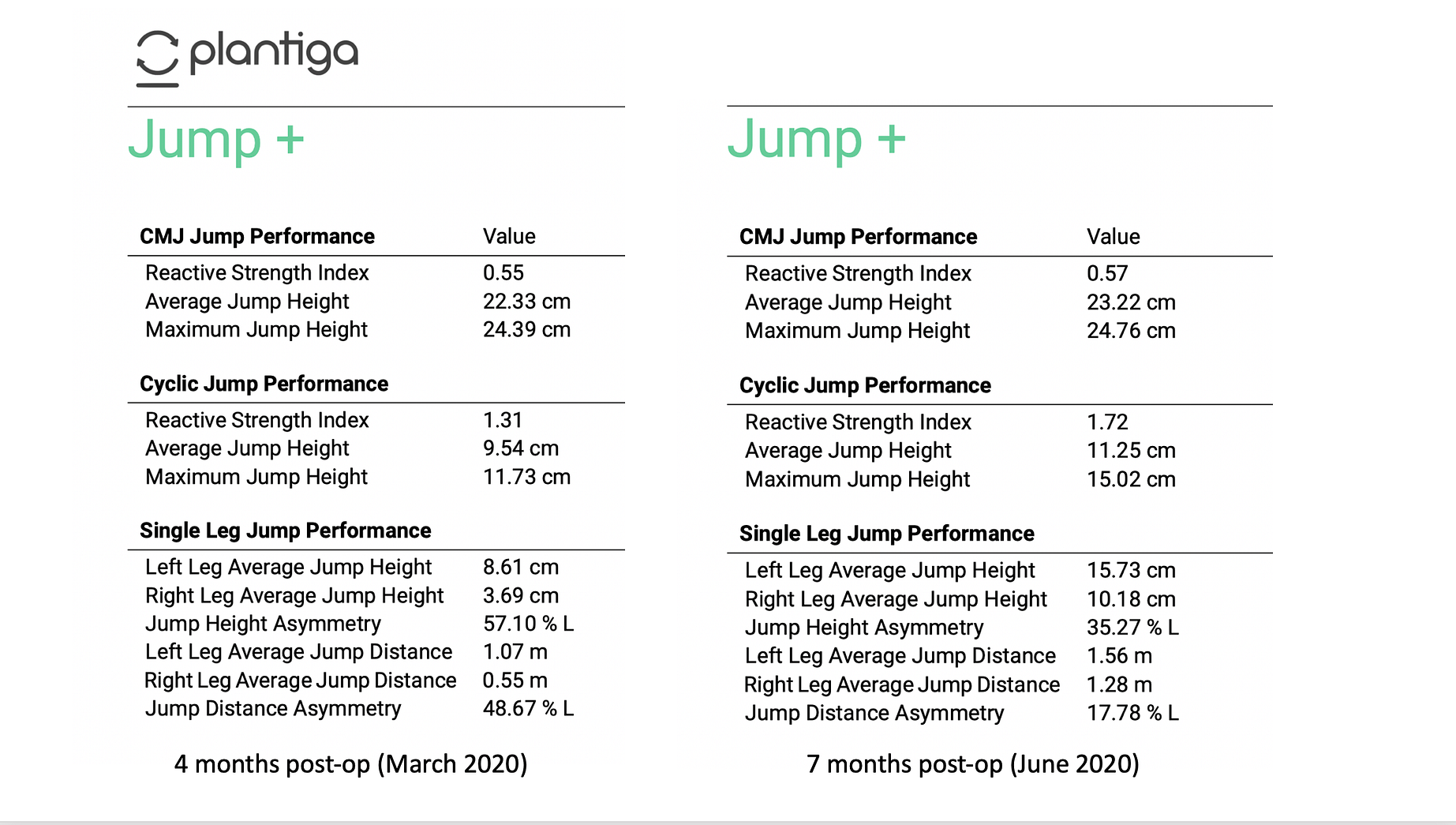
Plantiga Jump+ Reports
Sean’s jump data support Dr. Jordan’s concern that focusing on limb symmetry alone might miss the important functional deficits that remain after an injury both in the injured and non-injured limb. Sean’s jump height and distance asymmetries have drastically improved but look at the absolute values of distance and height for his left leg in March 2020, they were half of what they are now!
Sean’s focus on calf strengthening and plantar flexion range has resulted in marked improvement in his horizontal jumping ability. But, in my view, the reduced dorsiflexion range of motion limits his ability to get into a deep squat reducing his vertical jumping abilities in addition to the de-training he’s experienced. As a result, he has not yet returned to baseline with regard to his ability to generate dynamic power.
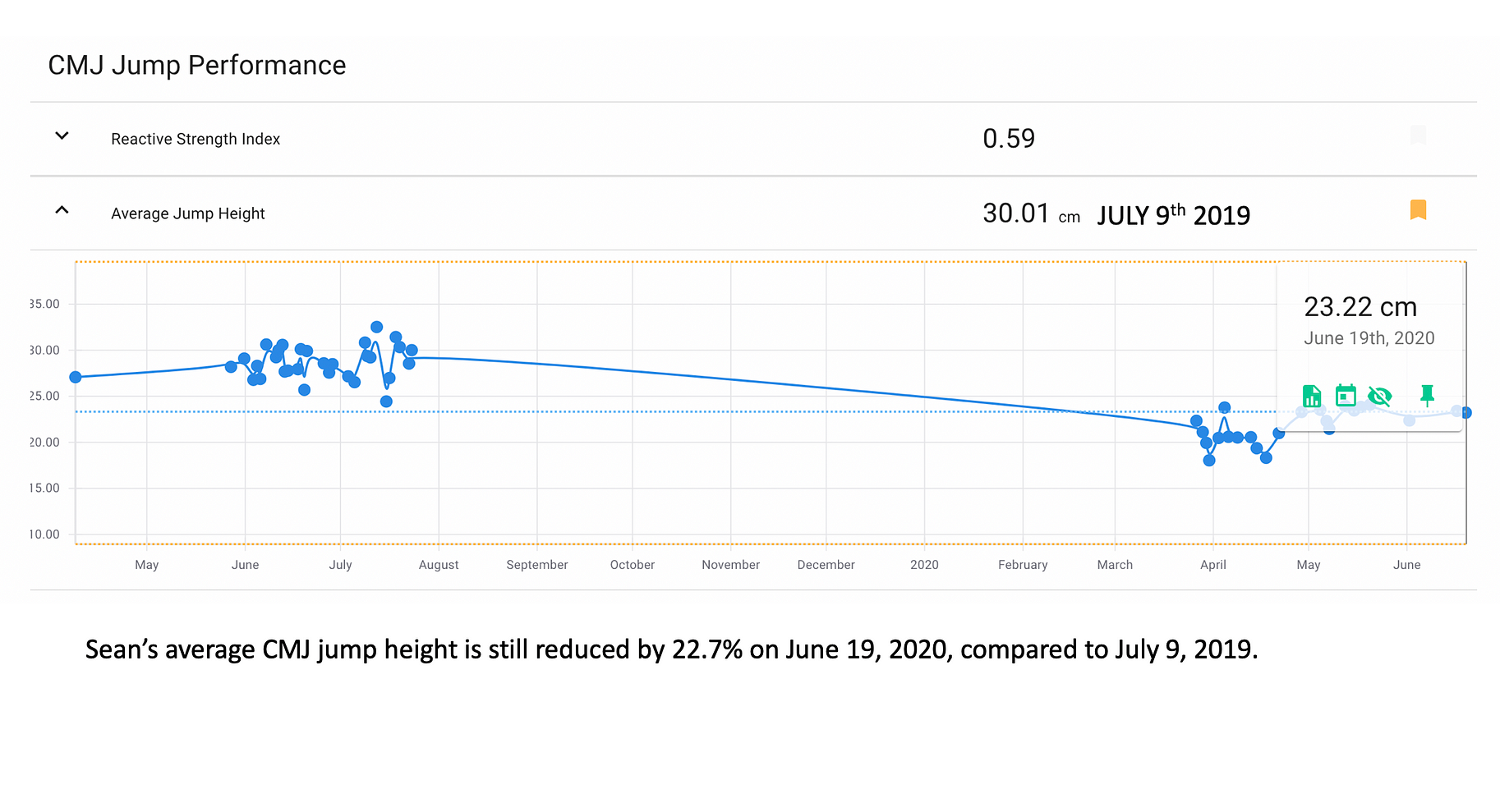
The deficit in dorsiflexion range doesn’t only limit Sean’s ability to generate power in the propulsion phase of jumping, it is also apparent in his landing which captures his eccentric weight acceptance ability.
The first image shows Sean’s CMJ performance in March 2020. Notice the deeper green spike (right limb) relative to the yellow (left limb). Eccentric G-Forces at impact are much higher in his injured limb which indicates he lacks the ability to absorb and dissipate forces at landing. This is likely another functional representation of his ankle stiffness.

The second image is from the same Plantiga jump test in June. Notice that on several jumps his G-forces at landing are symmetric while for others, the right remains higher in keeping with the ongoing stiffness he continues to report.
Plantiga Run Data
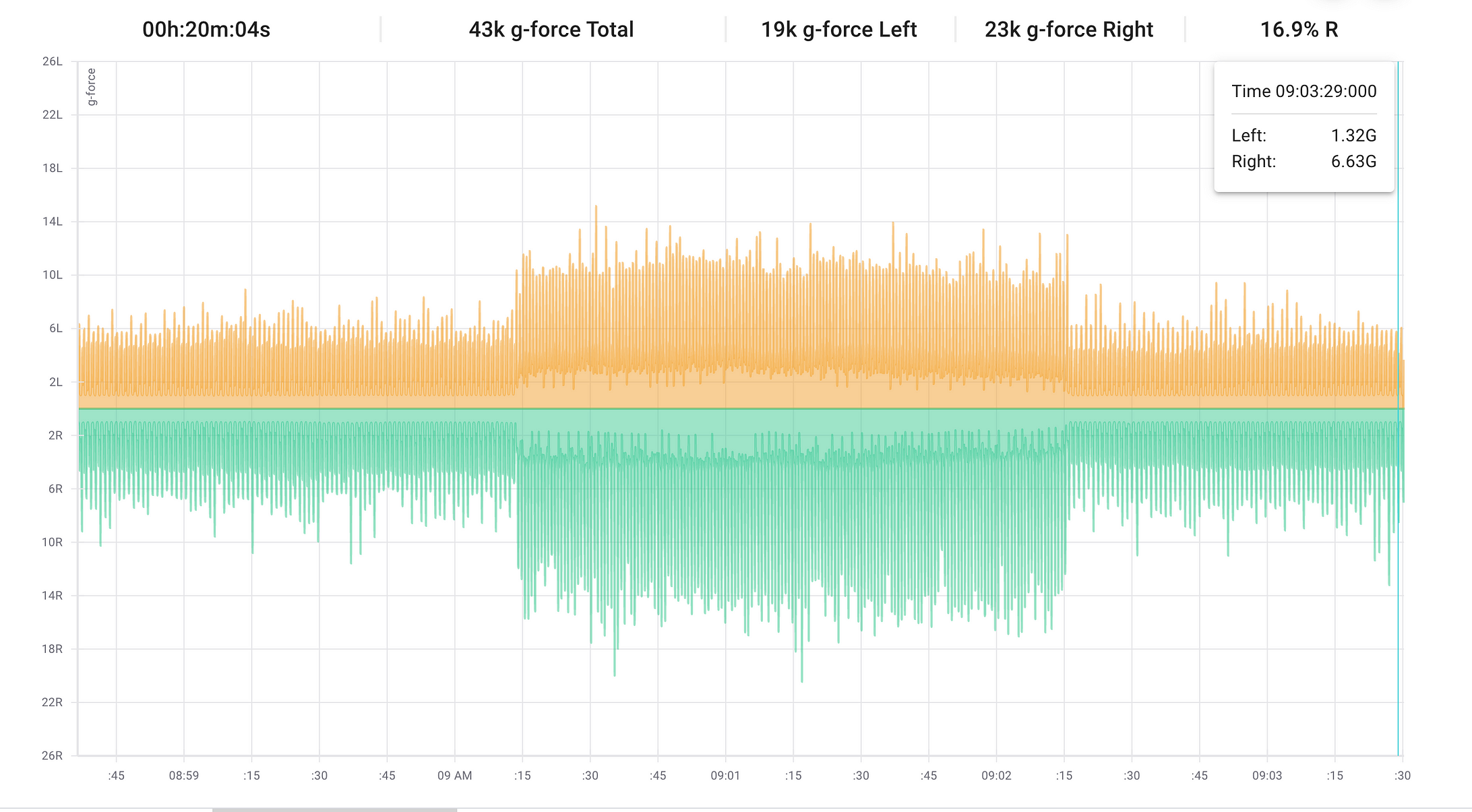
Plantiga Run G-Force Intensity — Raw Data
It appears that Sean’s jump trends carry over to running. This is not surprising since running is essentially a series of jumps. This is data from a recent run-walk workout Sean captured June 23, 2020. You can see that the green spikes on the bottom representing the G-Force accelerations of the right limb are much higher than the left on the top (both in walking — shorter bars and running — longer bars). The variability of the signal is also increased on the right relative to the left. I hypothesize that this finding is capturing the proprioceptive deficits that occur after injury. More research into this area would flush out important functional measures to capture as part of return to activity assessment.
Summary
Overall Sean is on the right track with his rehabilitation, but it’s slow. He has shown good recovery in the strength of his ankle complex on the right side reflecting what his rehabilitation has largely focused on. His walking has normalized. He is back to running but in a reduced capacity. Now from the Plantiga data it appears he is still dealing common secondary sequelae of a significant ankle injury requiring surgery and prolonged immobilization: stiffness and proprioceptive loss. This has resulted in both a loss of dynamic propulsive and weight acceptance ability in jumping and greater limb variability in higher intensity tasks like running.
My recommendations to Sean included more aggressive calf stretching including modalities like intramuscular stimulation (IMS) or myofascial trigger point release to facilitate this. Ultimately significant ankle injuries requiring surgical fixation often do lead to stiffness long term. I wonder if he might find running more comfortable with a shoe with a rocker sole to assist with weight acceptance in early stance. I’ve also suggested he try to use the right limb as much as possible: go down stairs leading with that side, put that foot down on the floor first getting out of bed or up from a chair in keeping with a constraint-led rehabilitation approach for limb asymmetries (more on asymmetries here). I’ve encouraged him to re-engage with a therapist that can guide him through more dynamic rehabilitation activities.
Plantiga offers unique insights that typical clinic tests can’t, especially during dynamic movements like jumping and running. More research is needed as to whether these differences predict the likelihood of return to sport and risk of re-injury. Plantiga is looking for research collaborations. Reach out to them if you’re interested in testing their product, using it in your laboratory or incorporating it in your return to activity protocols.
Guest Author - Dr. Kaila Holtz is a Physiatrist based in Vancouver, Canada. She specializes in musculoskeletal pain, osteoarthritis management, overuse sports or occupational injuries (e.g. running, pitching, sitting). She is the Medical Director of Triumph Health and Chief Medical Officer at Plantiga. When not in the clinic she is chasing her toddler and training for a half-marathon. Find her on Twitter @kailaholtz.
References
Zhang, P., Liang, Y., He, J. et al. A systematic review of suture-button versus syndesmotic screw in the treatment of distal tibiofibular syndesmosis injury. BMC Musculoskelet Disord 18, 286 (2017). https://doi.org/10.1186/s12891-017-1645-7
John D Johnson, Laura A Chachula, Ryan J Bickley, Claude D Anderson, Paul M Ryan, Return to Duty Following Open Reduction and Internal Fixation of Unstable Ankle Fractures in the Active Duty Population, Military Medicine, Volume 184, Issue 5–6, May-June 2019, Pages e381–e384, https://doi.org/10.1093/milmed/usy325
Loeffen, F. G. J., Shimozono, Y., Kerkhoffs, G. M. M. J., & Kennedy, J. G. (2018). Return to Play After Ankle Injuries BT — Return to Play in Football: An Evidence-based Approach (V. Musahl, J. Karlsson, W. Krutsch, B. R. Mandelbaum, J. Espregueira-Mendes, & P. d’Hooghe (eds.); pp. 365–386). Springer Berlin Heidelberg. https://doi.org/10.1007/978-3-662-55713-6_29
Hunt KJ, Phisitkul P, Pirolo J, Amendola A (2015) High ankle sprains and syndesmotic injuries in athletes. J Am Acad Orthop Surg 23(11):661–673
